E-Mail: sales@microapproachmed.com
Phone: +86-17722685792
- All
- Product Name
- Product Keyword
- Product Model
- Product Summary
- Product Description
- Multi Field Search
E-Mail: sales@microapproachmed.com
Phone: +86-17722685792
Views: 0 Author: Site Editor Publish Time: 2026-02-04 Origin: Site








Urology includes many procedures, but one appears more often than others.
Patients, clinicians, and buyers often ask which surgery dominates daily practice.The answer affects training, planning, and Urology equipment decisions.“Most common” usually reflects real hospital demand, not theory.In this article, you will learn which surgery leads urology practice.
When people ask for the most common urology surgery, they often mix two ideas: the procedure done most frequently and the procedure with the highest clinical stakes. These are not the same, because a rare cancer surgery can be highly important yet performed far less often than a routine procedure for a widespread condition. Volume reflects repeat demand, predictable scheduling, and ongoing referrals, while clinical importance reflects severity, progression risk, and long-term outcomes. For you, volume tends to matter more for planning, because it predicts how often staff will use Urology equipment, how quickly consumables will turn, and how frequently preventive maintenance must occur.
Urology includes many office-based procedures that occur at high frequency, but they often require limited equipment and short recovery times. Hospital-based surgeries typically involve operating room time, anesthesia services, and more complex equipment stacks, so they carry greater operational impact even if their absolute case count is lower than quick outpatient tests. When a hospital asks “most common surgery,” they usually mean the most common procedure that repeatedly consumes operating room resources, nursing workflows, sterile processing capacity, and a consistent set of Urology equipment components.
Urology demand strongly correlates with age, because conditions like benign prostatic hyperplasia, urinary obstruction, and recurrent stone disease increase as populations age. This means that even if clinical guidelines evolve, baseline demand often remains strong due to demographics alone. In many regions, the male population over fifty drives a large share of surgical and procedural volume, and that demand tends to rise steadily as life expectancy increases. If you are planning service growth or product supply, the demographic signal is often stronger than short-term trend signals, although exact prevalence figures can vary by country and dataset (validation required).
Clinical preference is not purely theoretical, because surgeons tend to choose procedures that fit the facility’s capabilities and that can be delivered safely at scale. Equipment availability matters, because standardized platforms shorten learning curves, simplify credentialing, and reduce the risk of delays caused by missing instruments or inconsistent accessories. Hospitals also prefer procedures that match current inventory and service contracts, because they reduce capital burden and simplify maintenance planning. In practice, the “most common” surgery often becomes the one best supported by existing Urology equipment and repeatable workflows, not merely the one that looks most advanced on paper.
Across many inpatient urology services, Transurethral Resection of the Prostate (TURP) is widely recognized as the most commonly performed urology surgery, because it treats urinary obstruction caused by benign prostate enlargement and it has a long-established technical pathway. TURP is performed through the urethra using an endoscopic approach, which avoids external incisions and allows surgeons to remove obstructive tissue under direct visualization. From a systems perspective, TURP also benefits from mature training resources, standardized instrumentation, and stable perioperative protocols, which is why it remains a core procedure in many hospitals even as alternative technologies expand.
BPH is common in aging men and often causes lower urinary tract symptoms that worsen over time, such as weak stream, hesitancy, nocturia, urgency, and incomplete emptying. Medication and lifestyle changes can reduce symptoms for many patients, but progression and treatment failure still occur, especially when obstruction becomes significant. When symptoms persist and quality of life declines, surgery becomes a practical next step, and TURP often remains a default choice because it is widely available and because outcomes are relatively predictable across skilled teams. In volume terms, BPH creates a steady referral pipeline rather than a seasonal spike, which supports consistent OR scheduling and consistent demand for Urology equipment tied to resection and fluid management.
Vasectomy is very common in outpatient settings and can appear frequently in clinic logs, but it serves a narrower population and it usually requires fewer hospital resources. TURP, in contrast, targets a widespread age-linked condition and frequently requires operating room resources, anesthesia, and inpatient or short-stay recovery protocols. In other words, vasectomy may dominate office counts in some markets, while TURP often dominates hospital surgical demand, which matters more for facility planning, equipment procurement, and service contracts. If you are modeling operational load or equipment needs, you should separate office procedure counts from inpatient surgery volume (validation required for local datasets).
Across typical urology service lines, TURP consistently appears among the top surgeries scheduled in OR blocks, particularly in facilities that manage a large older male population. You will also see related prostate interventions performed frequently, but TURP remains a reference standard in many regions because it is supported by established training and equipment ecosystems. Exact rankings can shift depending on local practice patterns, payer systems, and access to newer technologies, so it is best to validate with your facility’s coding and case mix data, but the overall trend remains stable across many settings (validation required).
The main reason TURP remains dominant is simple: the patient pool is large and persistent, because BPH increases with age and many patients eventually reach a point where medication is insufficient. This creates a long, predictable curve of demand that supports stable staffing models and repeatable surgical scheduling, and it also simplifies forecasting for sterile processing, scopes, and electrosurgical support. For hospitals, the “steady pipeline” matters because it reduces idle OR time, while for suppliers it creates a consistent baseline for replacement parts and compatible accessories within the Urology equipment stack.
TURP has a long clinical history, so teams understand typical risks and recovery patterns, and hospitals have standardized patient pathways that reduce variability. Predictability matters for quality metrics, because it supports consistent counseling, consistent post-op monitoring, and consistent discharge criteria. From a B2B view, predictable pathways support consistent consumption of disposables and consistent service schedules for resectoscopes and energy platforms, which reduces total operating risk. Facilities often prefer “well-known” procedures when they need high throughput and stable outcomes, even if they also offer newer options for selected patients.
Because TURP is endoscopic, it avoids large external incisions, which can reduce tissue trauma and shorten recovery compared with open approaches in appropriate cases. Many patients can return to basic activities relatively quickly, and hospitals often see shorter length of stay compared with more invasive surgery types, depending on comorbidities and local protocols (validation required). That operational efficiency supports patient flow, improves bed availability, and reduces downstream costs, which helps explain why TURP remains widely practiced even as laser and other methods continue to develop.
Standardization is a quiet driver of dominance, because TURP depends on a stable set of devices: resectoscopes, visualization, energy generators, irrigation, and safety monitoring. Most hospitals have long experience maintaining these systems, and most surgical staff already know the workflows, which reduces training time and lowers the risk of procedural delays. When a procedure aligns with existing equipment and training, it scales faster and it remains durable over time, which is exactly what we see with TURP in many urology departments.
Resectoscopes are central to TURP because they provide endoscopic access through the urethra while supporting tissue resection under direct visualization. They typically integrate optical pathways, working channels, and attachments that allow surgeons to cut and coagulate tissue, and image clarity directly affects precision. Visualization systems, including camera heads and monitors, also influence workflow, because clear imaging reduces hesitation and improves control, especially when tissue planes are subtle. In procurement terms, resectoscopes and visualization gear represent core capital Urology equipment that must be supported by maintenance schedules, spare parts planning, and consistent cleaning protocols.
Energy platforms supply the cutting and coagulation power required for resection, and output stability affects bleeding control and operative efficiency. Consistent energy delivery supports predictable tissue effects, while poor stability can increase time, increase bleeding, and increase stress for the surgical team. Because these units often serve multiple specialties, urology teams typically rely on standardized settings and shared safety protocols, which strengthens the value of clear training and reliable vendor support. For B2B readers, energy equipment is not only a clinical choice; it is also a service choice, because uptime and calibration schedules directly affect OR performance.
Irrigation supports visibility by clearing blood and debris, and fluid management helps maintain safe pressures and volumes throughout the procedure. Safety monitoring tools help teams track key parameters that reduce risk during prolonged endoscopic work, including attention to fluid balance and patient stability. These systems rarely appear in marketing headlines, but they often determine whether a procedure feels smooth or chaotic, and they influence complication risk. In practice, these components form an essential “support layer” of Urology equipment that should be planned as a system, not as isolated purchases.
Even though TURP is the most common urology surgery in many hospitals, daily urology work includes frequent minimally invasive kidney and ureter interventions, and these cases rely on precise accessory devices that often have high turnover. Guidewires support safe access and navigation through urinary anatomy, ureteral stents help maintain drainage and reduce obstruction risk after intervention, and stone baskets help retrieve fragments during ureteroscopy. Manufacturers such as Shenzhen MicroApproach Medical Technology Co., Ltd. focus on these devices because they directly support precision and safety in high-frequency minimally invasive workflows, and they can help teams reduce procedural variability across different operators and patient anatomies. When you evaluate Urology equipment needs, these “smaller” tools often drive recurring spend and can strongly influence case efficiency.
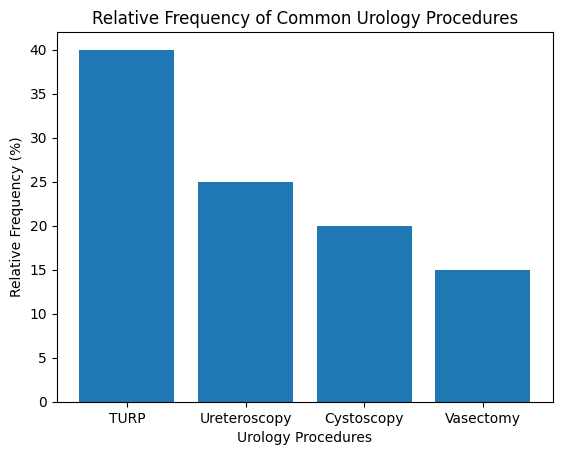
Cystoscopy is one of the most common urology procedures overall, but it is frequently diagnostic and often performed in office or outpatient settings. TURP, by contrast, is a definitive surgical treatment that usually requires an operating room setup, anesthesia coordination, and a deeper equipment stack. This distinction matters for B2B readers, because diagnostic volume can be high while resource intensity remains low, whereas TURP volume can be slightly lower in raw counts but far higher in equipment use, sterile processing load, and OR scheduling impact. When you compare “common procedures,” you should compare like with like: diagnostic procedures vs surgical procedures, and outpatient vs inpatient resource profiles.
Ureteroscopy is widely used for stone diagnosis and removal, and it depends heavily on endoscopic navigation and retrieval tools, including guidewires and baskets. Its volume can fluctuate based on population habits, hydration patterns, and regional factors, whereas BPH-driven TURP demand often remains stable due to age-linked prevalence. From an equipment perspective, ureteroscopy can be consumable-heavy, especially when cases require multiple guidewires, stents, or retrieval devices. This is one reason why portfolios like Shenzhen MicroApproach’s focus on those devices, because steady stone case flow can generate consistent recurring demand for these products within the broader Urology equipment ecosystem.
Vasectomy is common in office-based care and is often done as a short procedure with a limited equipment footprint. TURP requires more staff coordination and more complex instrumentation, so it carries a larger “operations and equipment” footprint per case. If your organization measures volume as “number of procedures,” vasectomy may look dominant in some clinic datasets, but if you measure volume as “surgical time, equipment usage, and inpatient impact,” TURP often becomes the clear leader. This is why hospitals often treat TURP as a core service line procedure, while clinics may treat vasectomy as a high-volume outpatient offering.
The difference between procedures becomes clearer when you compare resource intensity rather than counting cases, because equipment needs and turnover patterns differ significantly across urology categories.
Procedure category | Typical clinical goal | Core Urology equipment drivers | Planning impact |
TURP | Relieve obstruction from BPH | Resectoscope, energy system, irrigation, fluid monitoring | OR time, capital maintenance, standardized pathways |
Ureteroscopy | Diagnose or remove stones | Ureteroscope, guidewires, stents, stone baskets | Consumable turnover, inventory forecasting |
Cystoscopy | Inspect bladder and urethra | Cystoscope, camera, basic irrigation | High volume, lower intensity per case |
Vasectomy | Permanent male contraception | Basic surgical tools, local anesthesia supplies | High outpatient volume, low equipment intensity |
Several alternatives to TURP exist, including laser-based prostate treatments, and these options may offer advantages for selected patient groups or specific clinical goals. Adoption varies across regions because the equipment costs, training requirements, and reimbursement rules differ widely, and some facilities prioritize broader access over specialization. TURP often remains the practical baseline because it is widely available and because its workflows are familiar across many teams. For B2B readers, this does not mean alternatives are unimportant; it means you should align technology adoption with case volume, staffing, and service support realities.
Technology improvements often reduce length of stay indirectly by improving intraoperative control and reducing post-op complications. Better optics can shorten decision time and reduce uncertainty, while improved energy control can reduce bleeding and improve hemostasis. More reliable irrigation and fluid management can reduce procedural stress and help teams maintain safe operative conditions. These upgrades usually strengthen existing procedures rather than replacing them, so many facilities invest in incremental improvements to familiar equipment stacks to raise throughput and reduce complications.
Robotic systems have grown rapidly in urologic oncology, but their role in benign prostate surgery varies widely. Costs remain high, and training requirements are substantial, so adoption depends on patient mix, surgical leadership, and capital budgets. For benign conditions, many facilities still prefer the accessibility and standardization of TURP because it fits existing Urology equipment capabilities and because it supports predictable throughput. Over time, market shifts may change relative shares, but “dominant today” is still driven by access, affordability, and operational repeatability.
Even when a technology looks superior on paper, adoption can stall if training is complex or if ongoing costs are unclear. Hospitals and ambulatory centers need devices that work reliably across many operators, and they need supply chains that can support consistent case flow. This is where accessory device providers matter, because guidewires, stents, and baskets must be consistently available and consistent in performance to avoid workflow disruptions. If a facility cannot guarantee device availability, the “best” technique can become the least practical technique in real operations.
TURP remains a core investment area because it supports predictable case demand tied to demographics, and it often anchors a facility’s benign urology surgical service line. Predictable utilization improves return on capital equipment and simplifies long-term service contracting. Because TURP equipment stacks are standardized, hospitals can train staff more efficiently and maintain consistent quality metrics across many surgeons. This is why TURP-related Urology equipment typically remains on replacement and upgrade plans even when new technologies are introduced.
High-volume equipment requires disciplined preventive maintenance, because minor failures can quickly create cancellations and reduce OR throughput. Staff training must also remain consistent, especially in settings with turnover across nursing and sterile processing roles. Standardized checklists, clear setup routines, and reliable vendor support reduce downtime and lower the risk of workflow variation. In the long run, maintenance planning is not a “support task,” because it directly affects patient access and revenue stability.
Supply chain stability is especially important in urology because many procedures require both reusable and disposable components, and missing a small disposable item can stall an entire case. Consumables like guidewires, ureteral stents, and stone baskets often follow predictable demand patterns based on ureteroscopy volume, and they can represent a meaningful share of recurring spend. Companies like Shenzhen MicroApproach Medical Technology Co., Ltd. support this demand by offering a lineup of minimally invasive urology devices that align with routine kidney and ureter interventions, which helps facilities reduce vendor fragmentation and stabilize inventory planning.
Future-proofing usually means building modularity rather than chasing one “final” platform, because clinical practice evolves and budgets remain constrained. Scalable procurement strategies often include selecting systems with broad compatibility, maintaining a balanced mix of capital equipment and consumables, and ensuring supplier continuity for frequently used devices. In practical terms, a department that supports TURP well while also maintaining consistent access to guidewires, stents, and baskets can deliver stable service across both prostate and stone pathways. This balanced approach often aligns better with real patient demand and creates resilience in the Urology equipment ecosystem.
Stakeholder | What “most common” implies | What to prioritize in Urology equipment |
Hospitals | Stable OR scheduling and throughput | Standardized TURP stack, preventive maintenance, inventory controls |
Clinics | High outpatient volume, fast turnover | Reliable diagnostic scopes, streamlined supply kits |
Distributors | Predictable recurring demand | Consistent supply of guidewires, stents, baskets, plus service parts |
Manufacturers | High-use product categories | Safety, tactile control, compatibility, documented performance |
A practical urology equipment plan combines durable capital systems with reliable high-turn consumables.
When you ask, what is the most common urology surgery, the most practical answer in many hospitals remains Transurethral Resection of the Prostate (TURP), because BPH is common, progression is predictable, and clinical workflows are standardized. TURP also stays dominant because it fits established training pathways and aligns with existing Urology equipment stacks, including resectoscopes, energy platforms, irrigation systems, and safety monitoring tools. At the same time, modern urology care is not limited to TURP, because minimally invasive kidney and ureter interventions also occur frequently and rely on precision devices such as guidewires, ureteral stents, and stone baskets. Suppliers like Shenzhen MicroApproach Medical Technology Co., Ltd. contribute to these workflows by providing devices designed for precision and safety, which can support smoother interventions and more predictable case efficiency. For patients, this understanding clarifies why TURP appears so often in care pathways, while for hospitals and B2B buyers it provides a clear foundation for planning, purchasing, and scaling a urology service line.
A: Transurethral resection of the prostate is the most common urology surgery because it treats benign prostatic hyperplasia using standardized Urology equipment in routine hospital practice.
A: Prostate enlargement affects many aging men, and reliable Urology equipment allows surgeons to perform this procedure safely and efficiently at high volume.
A: Key Urology equipment includes resectoscopes, electrosurgical generators, irrigation systems, and monitoring tools that ensure precision and patient safety.
A: Costs remain predictable, and recovery is shorter than open surgery due to minimally invasive techniques and established clinical workflows.
14 Jinhui Road, Pingshan District, Shenzhen,518122, P.R.China
+86-755-89459010
+86-18320758765 Ares
+86-15013496274 Daisy
+86-15813727825 Gloria